The life and times of a pituitary Cushing's survivor (1987) AND a kidney cancer (Renal Cell Carcinoma) survivor (2006). I must be a Super-Woman...NOT!
Saturday, March 31, 2012
It's HERE! The Cushing's Awareness Challenge

Enjoy following the posts of these outstandingly brave Cushies as they attempt to post a blog post each day for the month of April
Amber http://amber-mulnix.blogspot.com/
Christina http://christinapay.blogspot.com/Cristina (Portugese language) http://cristinagoncalves1973.blogspot.pt/Danielle http://lifewithcushings.blogspot.com/DawnGrace C http://adayinthelifeofatrainwreck.blogspot.com/Judy DKay http://cushiemama.blogspot.com Lisa DMalia KMary BMaryO http://www.cushie.info/blog/Melissa AMelissa SMissaf http://blogforacushiecure.blogspot.com/Molli http://livingwithstripes.blogspot.com/Nancy J http://cushielife.multiply.com/Rene B http://missdiagnosis-rene.blogspot.com/Robin S survivethejourney.blogspot.comSarah C http://sarahsstupiddisease.wordpress.com/Sharon SShermaineStanley LStephanie Y cushiesteph.blogspot.comTrishaVanessa http://www.blogger.com/profile/05094821916178382160
Enjoy!

Friday, March 30, 2012
Thursday, March 29, 2012
A classification tree approach for pituitary adenomas
- Alberto Righi, MD ,
- Patrizia Agati, BSI, PhD ,
- Andrea Sisto, BSI ,
- Giorgio Frank, MD ,
- Marco Faustini-Fustini, MD ,
- Raffaele Agati, MD ,
- Diego Mazzatenta, MD ,
- Anna Farnedi, BSc, PhD ,
- Federico Menetti, MD ,
- Gianluca Marucci, MD ,
- Maria P. Foschini, MD


Summary
It is difficult to evaluate the recurrence and progression potential of pituitary adenomas at presentation. The World Health Organization classification of endocrine tumors suggests that invasion of the surrounding structures, size at presentation, an elevated mitotic index, a Ki-67 labeling index higher than 3%, and extensive p53 expression are indicators of aggressive behavior.
Nevertheless, Ki-67 and p53 labeling index evaluation is subject to interobserver variability, and their cutoff values are controversial. In the present study, the prognostic value of Ki-67 and p53 protein labeling indices and their correlation with clinical and radiologic parameters were evaluated using digital image analysis in a series of 166 pituitary adenomas in patients having undergone a follow-up of at least 6 years to evaluate the impact on the recurrence and progression potential of pituitary adenomas.
The data were analyzed using the receiver operating characteristic curve and classification and regression tree analysis. The results showed that, in the unstratified data set, the commonly used threshold of the Ki-67 index of 3% has a high specificity (89.5%) but a low sensitivity (53.8%).
Unsatisfactory performance results were obtained by performing receiver operating characteristic curve analysis on the p53 labeling index. On the contrary, the classification and regression tree analysis–derived tree demonstrated that each pituitary adenoma subtype has specific prognostic factors.
Specifically, the Ki-67 labeling index is a useful prognostic factor in nonfunctioning, adrenocorticotropin, and prolactin adenomas, but with different thresholds. In conclusion, our study emphasizes that the term pituitary adenomas includes different types of tumors, each one having specific prognostic factors.
Access the entire article here: http://www.humanpathol.com/article/PIIS0046817711004965/abstract?rss=yes
Cushing's Awareness Challenge Countdown...
Only 3 days (counting today) until the Cushing's Awareness Challenge begins. At night, when I'm supposed to be sleeping, ideas for posts keep swarming through my head. Sometimes, they form into fully-written posts. Then, when I wake up, the posts are gone.
I plan to follow the suggestions to some extent and have a few ideas of my own. Over the years, I've posted lots on several blogs but I don't know if I can get 30 days of Cushing's stuff together!
At the moment, there are 26 participants in this challenge and growing. Please follow their blogs. The list is here and is constantly updated as new URLs come in.
If you want to join us, its not too late. Directions and suggestions for posts can be found here: http://cushie-blogger.blogspot.com/2012/03/cushing-awareness-challenge.html
If you have ideas for what you'd like to read about (Cushing's related, of course), please feel free to put it in the comments area.
Wednesday, March 28, 2012
PharmaForm announces commercial manufacturing contract for Corcept's Korlym™
PharmaForm announced that Corcept Therapeutics Inc. has chosen PharmaForm as their primary commercial manufacturer for their newly approved drug product, Korlym™. The U.S. Food and Drug Administration approved Corcept's Korlym™ on February 17th, 2012 for patients with endogenous Cushing's syndrome.
PharmaForm, a full-service contract provider of development and manufacturing for the pharmaceutical and biotech industry, has worked with Corcept for several years as a contract provider for services in the development, optimization and validation of the manufacturing process for Corcept's Korlym™.
Read the entire article here: http://www.marketwatch.com/story/pharmaform-announces-commercial-manufacturing-contract-for-corcepts-korlym-2012-03-26
Tuesday, March 27, 2012
Cushing's Awareness Challenge
Do you blog? Want to get started?
Since April 8 is Cushing's Awareness Day, several people got their heads together to create this blogging challenge.
All you have to do is blog about something Cushing's related for the 30 days of April. Robin designed 3 versions of our "official logo" to put on your blogs.
Please note that these are thumbnails - the actual image is larger than shown here. Click on the images to view actual size.
If your blog wants you to upload an image from your desktop, right-click on the image above and choose "save-as". Remember where you saved it to!
In all cases, the URL for the site is http://www.cushings-help.com
[[posterous-content:pid___0]]Small. If your blog asks you to enter the URL, use this:

Medium. If your blog asks you to enter the URL, use this:

Large. If your blog asks you to enter the URL, use this:

Please let me know the URL to your blog and I will list it on CushieBloggers ( http://cushie-blogger.blogspot.com/ ) The more people who participate, the more the word will get out about Cushing's.
Suggested topics - or add your own!
- In what ways have Cushing's made you a better person?
- What have you learned about the medical community since you have become sick?
- If you had one chance to speak to an endocrinologist association meeting, what would you tell them about Cushing's patients?
- What would you tell the friends and family of another Cushing's patient in order to garner more emotional support for your friend? challenge with Cushing's? How have you overcome challenges? Stuff like that.
- I have Cushing's Disease....(personal synopsis)
- How I found out I have Cushing's
- What is Cushing's Disease/Syndrome? (Personal variation, i.e. adrenal or pituitary or ectopic, etc.)
- My challenges with Cushing's
- Overcoming challenges with Cushing's (could include any challenges)
- If I could speak to an endocrinologist organization, I would tell them....
- What would I tell others trying to be diagnosed? What would I tell families of those who are sick with Cushing's?
- Treatments I've gone through to try to be cured/treatments I may have to go through to be cured.
- What will happen if I'm not cured?
- I write about my health because…
- 10 Things I Couldn’t Live Without.
- My Dream Day.
- What I learned the hard way
- Miracle Cure. (Write a news-style article on a miracle cure. What’s the cure? How do you get the cure? Be sure to include a disclaimer)
- Health Madlib Poem. Go to : http://languageisavirus.com/cgi-bin/madlibs.pl and fill in the parts of speech and the site will generate a poem for you.
- The Things We Forget. Visit http://thingsweforget.blogspot.com/ and make your own version of a short memo reminder. Where would you post it?
- Give yourself, your condition, or your health focus a mascot. Is it a real person? Fictional? Mythical being? Describe them. Bonus points if you provide a visual!
- 5 Challenges & 5 Small Victories.
- The First Time I…
- Make a word cloud or tree with a list of words that come to mind when you think about your blog, health, or interests. Use a thesaurus to make it branch more.
- How much money have you spent on cushing's, or, How did Cushing's impact your life financially?
- Why do you think Cushing's may not be as rare as doctors believe?
- What is your theory about what causes Cushing's?
- How has Cushing's altered the trajectory of your life? What would you have done? Who would you have been?
- What three things has Cushing's stolen from you? What do you miss the most? What can you do in your Cushing's life to still achieve any of those goals? What new goals did Cushing's bring to you?
- How do you cope?
- What do you do to improve your quality of life as you fight Cushing's?
- Your thoughts...?
Monday, March 26, 2012
Cushing's Awareness Challenge
Do you blog? Want to get started?
Since April 8 is Cushing's Awareness Day, several people got their heads together to create this blogging challenge.
All you have to do is blog about something Cushing's related for the 30 days of April. Robin designed 3 versions of our "official logo" to put on your blogs.
Please note that these are thumbnails - the actual image is larger than shown here. Click on the images to view actual size.
If your blog wants you to upload an image from your desktop, right-click on the image above and choose "save-as". Remember where you saved it to!
In all cases, the URL for the site is http://www.cushings-help.com
Small. If your blog asks you to enter the URL, use this:
Medium. If your blog asks you to enter the URL, use this:

Large. If your blog asks you to enter the URL, use this:

Please let me know the URL to your blog and I will list it on CushieBloggers ( http://cushie-blogger.blogspot.com/ ) The more people who participate, the more the word will get out about Cushing's.
Suggested topics - or add your own!
- In what ways have Cushing's made you a better person?
- What have you learned about the medical community since you have become sick?
- If you had one chance to speak to an endocrinologist association meeting, what would you tell them about Cushing's patients?
- What would you tell the friends and family of another Cushing's patient in order to garner more emotional support for your friend? challenge with Cushing's? How have you overcome challenges? Stuff like that.
- I have Cushing's Disease....(personal synopsis)
- How I found out I have Cushing's
- What is Cushing's Disease/Syndrome? (Personal variation, i.e. adrenal or pituitary or ectopic, etc.)
- My challenges with Cushing's
- Overcoming challenges with Cushing's (could include any challenges)
- If I could speak to an endocrinologist organization, I would tell them....
- What would I tell others trying to be diagnosed? What would I tell families of those who are sick with Cushing's?
- Treatments I've gone through to try to be cured/treatments I may have to go through to be cured.
- What will happen if I'm not cured?
- I write about my health because…
- 10 Things I Couldn’t Live Without.
- My Dream Day.
- What I learned the hard way
- Miracle Cure. (Write a news-style article on a miracle cure. What’s the cure? How do you get the cure? Be sure to include a disclaimer)
- Health Madlib Poem. Go to : http://languageisavirus.com/cgi-bin/madlibs.pl and fill in the parts of speech and the site will generate a poem for you.
- The Things We Forget. Visit http://thingsweforget.blogspot.com/ and make your own version of a short memo reminder. Where would you post it?
- Give yourself, your condition, or your health focus a mascot. Is it a real person? Fictional? Mythical being? Describe them. Bonus points if you provide a visual!
- 5 Challenges & 5 Small Victories.
- The First Time I…
- Make a word cloud or tree with a list of words that come to mind when you think about your blog, health, or interests. Use a thesaurus to make it branch more.
- How much money have you spent on cushing's, or, How did Cushing's impact your life financially?
- Why do you think Cushing's may not be as rare as doctors believe?
- What is your theory about what causes Cushing's?
- How has Cushing's altered the trajectory of your life? What would you have done? Who would you have been?
- What three things has Cushing's stolen from you? What do you miss the most? What can you do in your Cushing's life to still achieve any of those goals? What new goals did Cushing's bring to you?
- How do you cope?
- What do you do to improve your quality of life as you fight Cushing's?
- Your thoughts...?
Saturday, March 24, 2012
Korlym™ (mifepristone), the First Approved Medication for Patients with Endogenous Cushing’s Syndrome, to be Available by April 11
Corcept Therapeutics (NASDAQ:CORT) announced that it would be ready to ship Korlym to patients by April 11th, three weeks ahead of the company’s previously announced launch date. “Cushing’s syndrome is a life altering and life threatening disease,” said Joseph K. Belanoff, M.D., the company’s Chief Executive Officer. “We have worked hard to bring this first-in-class treatment to patients as quickly as possible.”
On February 17, 2012, the U.S. Food and Drug Administration (FDA) approved KorlymTM (mifepristone) 300 mg Tablets as a once-daily oral medicine to control hyperglycemia secondary to hypercortisolism in adult patients with endogenous Cushing’s syndrome who have type 2 diabetes mellitus or glucose intolerance and have failed surgery or are not candidates for surgery. Physicians and patients seeking more information can visit http://www.korlym.com.
Korlym is distributed in 300 milligram tablets to be taken once each day. The wholesale acquisition price of Korlym is $0.62 per milligram. The FDA-approved labeling instructs physicians to titrate each patient’s Korlym dose to clinical efficacy by assessing tolerability and degree of improvement in Cushing’s syndrome manifestations. In the first six weeks, these manifestations may include changes in glucose control, anti-diabetic medication requirements, insulin levels and psychiatric symptoms. After two months, assessment may also be based on improvements in cushingoid appearance, acne, hirsutism, striae or decreased body weight, along with further changes in glucose control.
Patient Assistance Programs
“Our highest priority is that every patient who is prescribed Korlym will receive it,” said Dr. Belanoff. To that end, the company has launched a comprehensive financial assistance and patient support program. A dedicated team of Corcept case managers will help patients understand their insurance benefits and the financial and medical support programs available to them.
“Patients face tremendous challenges managing their illness – from finding physicians familiar with the disease to navigating the complexities of insurance reimbursement to paying for the cost of care,” said Dr. Belanoff. “We are determined that none of these barriers will keep patients from receiving the benefits of Korlym.”
About Cushing’s Syndrome
Endogenous Cushing’s syndrome is a rare and life-threatening endocrine disorder that results from long-term exposure to excess levels of the hormone cortisol. This excess is caused by tumors that usually occur in the pituitary or adrenal glands that over-produce, or prompt the over-production of, cortisol.
Although cortisol at normal levels is essential to health, in excess it causes a variety of problems, including hyperglycemia, upper body obesity, a rounded face, stretch marks on the skin, an accumulation of fat on the back, thin and easily bruised skin, muscle weakness, bone weakness, persistent infections, high blood pressure, fatigue, irritability, anxiety, psychosis and depression. Women may have menstrual irregularities and facial hair growth, while men may have decreased fertility or erectile dysfunction. More than 70 percent of Cushing’s syndrome patients suffer from glucose intolerance or diabetes.
The treatment of an endogenous Cushing’s syndrome patient depends on the cause. The first-line approach is surgery to remove the tumor. If surgery is not successful or is not an option, radiation may be used, but that therapy can take up to ten years to achieve full effect. Surgery and radiation are successful in only approximately one-half of all cases.
If left untreated, Cushing’s syndrome has a five-year mortality rate of 50 percent.
An orphan disease, Cushing’s syndrome occurs in about 20,000 people in the United States, mostly women between the ages of 20 and 50.
About Korlym™ (mifepristone) 300 mg Tablets
Korlym is a once-daily oral medication that blocks the glucocorticoid receptor type II (GR-II) to which cortisol normally binds. By blocking this receptor, Korlym inhibits the effects of excess cortisol in Cushing’s syndrome patients.
The FDA has designated Korlym as an Orphan Drug, a special status designed to encourage the development of medicines for rare diseases and conditions. Because Korlym is an Orphan Drug, Corcept will have marketing exclusivity for the FDA-approved indication until February 2019.
IMPORTANT SAFETY INFORMATION
WARNING: TERMINATION OF PREGNANCY See full prescribing information for complete boxed warning.Mifepristone has potent antiprogestational effects and will result in the termination of pregnancy. Pregnancy must therefore be excluded before the initiation of treatment with Korlym, or if treatment is interrupted for more than 14 days in females of reproductive potential. |
Contraindications
- Pregnancy
- Use of simvastatin or lovastatin and CYP 3A substrates with narrow therapeutic range
- Concurrent long-term corticosteroid use
- Women with history of unexplained vaginal bleeding
- Women with endometrial hyperplasia with atypia or endometrial carcinoma
Warnings and Precautions
- Adrenal insufficiency: Patients should be closely monitored for signs and symptoms of adrenal insufficiency.
- Hypokalemia: Hypokalemia should be corrected prior to treatment and monitored for during treatment.
- Vaginal bleeding and endometrial changes: Women may experience endometrial thickening or unexpected vaginal bleeding. Use with caution if patient also has a hemorrhagic disorder or is on anti-coagulant therapy.
- QT interval prolongation: Avoid use with QT interval-prolonging drugs, or in patients with potassium channel variants resulting in a long QT interval.
- Use of Strong CYP3A Inhibitors: Concomitant use can increase plasma levels significantly. Use only when necessary and limit dose to 300 mg.
Adverse Reactions
Most common adverse reactions in Cushing’s syndrome (≥ 20%): nausea, fatigue, headache, decreased blood potassium, arthralgia, vomiting, peripheral edema, hypertension, dizziness, decreased appetite, endometrial hypertrophy.
To report suspected adverse reactions, contact Corcept Therapeutics at 1-855-844-3270 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Drugs metabolized by CYP3A: Administer drugs that are metabolized by CYP3A at the lowest dose when used with Korlym
- CYP3A inhibitors: Caution should be used when Korlym is used with strong CYP3A inhibitors. Limit mifepristone dose to 300 mg per day when used with strong CYP3A inhibitors.
- CYP3A inducers: Do not use Korlym with CYP3A inducers.
- Drugs metabolized by CYP2C8/2C9: Use the lowest dose of CYP2C8/2C9 substrates when used with Korlym.
- Drugs metabolized by CYP2B6: Use of Korlym should be done with caution with bupropion and efavirenz.
- Hormonal contraceptives: Do not use with Korlym.
Use in Specific Populations
- Nursing mothers: Discontinue drug or discontinue nursing.
Please see the accompanying full Prescribing Information including boxed warning atwww.corcept.com/prescribinginfo.pdf
Please see the accompanying Medication Guide at www.corcept.com/medicationguide.pdf
About Corcept Therapeutics Incorporated
Corcept is a pharmaceutical company engaged in the discovery, development and commercialization of drugs for the treatment of severe metabolic and psychiatric disorders. Korlym, a first generation GR-II antagonist, is the company’s first FDA-approved medication. The company has a portfolio of new selective GR-II antagonists that block the effects of cortisol but not progesterone. Corcept also owns an extensive intellectual property portfolio covering the use of GR-II antagonists, including mifepristone, in the treatment of a wide variety of psychiatric and metabolic disorders. The company also holds composition of matter patents for its selective GR-II antagonists.
Statements made in this news release, other than statements of historical fact, are forward-looking statements. Forward-looking statements are subject to a number of known and unknown risks and uncertainties that might cause actual results to differ materially from those expressed or implied by such statements. For example, there can be no assurances that clinical results will be predictive of real-world use, or regarding the pace of Korlym’s acceptance by physicians and patients, the reimbursement decisions of government or private insurance payers, the effects of rapid technological change and competition, the protections afforded by Korlym’s Orphan Drug Designation or by Corcept’s other intellectual property rights, and the cost, pace and success of Corcept’s other product development efforts. These and other risks are set forth in the Company's SEC filings, all of which are available from our website (www.corcept.com) or from the SEC's website (www.sec.gov). We disclaim any intention or duty to update any forward-looking statement made in this news release.
CONTACT:
Investor ContactCharles Robb
Chief Financial Officer
Corcept Therapeutics
650-688-8783
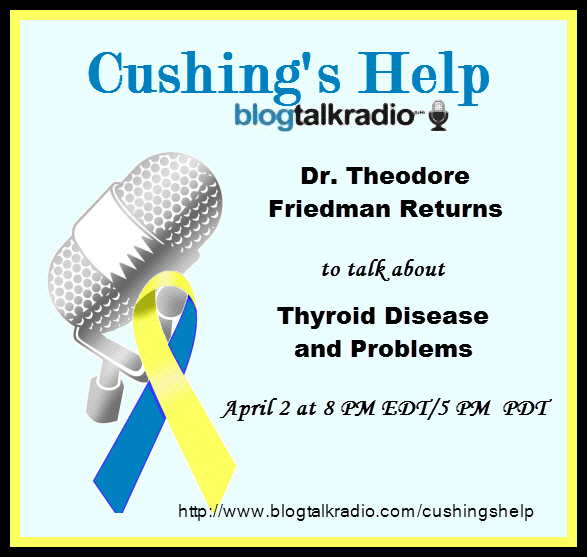
Dr. Theodore Friedman Will Return April 2
Ask Dr. Theodore Friedman.
Read Dr. Friedman's Second Guest Chat, March 2, 2004.
Listen to Dr. Friedman Second Live Voice Interview, March 12, 2009.
Listen to Dr. Friedman Third Live Voice Interview, February 13, 2011.
Listen to Dr. Friedman Fourth Live Voice Interview, March 12, 2012.
Dr. Theodore Friedman Will Return April 2
Have questions about thyroid issues?
Ask Dr. Theodore Friedman.
Theodore C. Friedman, M.D., Ph.D. has opened a private practice, specializing in treating patients with adrenal, pituitary, thyroid and fatigue disorders. Dr. Friedman has privileges at Cedars-Sinai Medical Center and Martin Luther King Medical Center. His practice includes detecting and treating hormone imbalances, including hormone replacement therapy. Dr. Friedman is also an expert in diagnosing and treating pituitary disorders, including Cushings disease and syndrome.
Dr. Friedman's career reflects his ongoing quest to better understand and treat endocrine problems. With both medical and research doctoral degrees, he has conducted studies and cared for patients at some of the country's most prestigious institutions, including the University of Michigan, the National Institutes of Health, Cedars-Sinai Medical Center, and UCLA's Charles Drew University of Medicine and Science.
Read Dr. Friedman's First Guest Chat, November 11, 2003.
Read Dr. Friedman's Second Guest Chat, March 2, 2004.
Listen to Dr. Friedman First Live Voice Interview, January 29, 2009.
Listen to Dr. Friedman Second Live Voice Interview, March 12, 2009.
Listen to Dr. Friedman Third Live Voice Interview, February 13, 2011.
Listen to Dr. Friedman Fourth Live Voice Interview, March 12, 2012.
Dr. Friedman will return April 2, 2012. The call in number with questions or comments is (646) 200-0162.
Listen live at http://www.blogtalkradio.com/cushingshelp
This interview will be archived afterwards at the same link and on iTunes Cushie Podcasts
Single-Incision Transperitoneal Laparoscopic Left Adrenalectomy
Óscar Vidal, Emiliano Astudillo, Mauro Valentini, Cesar Ginestà, Juan C. García-Valdecasas and Laureano Fernandez-Cruz
Abstract
Background
Laparoscopic adrenalectomy via three or four trocars is a well-established procedure. This report describes the initial experience with single-incision laparoscopic surgery (SILS) using the transperitoneal approach for left adrenalectomy.
Methods
Between April 2010 and August 2011, all consecutive patients with adrenal masses, including Conn’s syndrome, Cushing’s adenoma, and nonfunctional adrenal tumors, who agreed to undergo SILS adrenalectomy were included in a prospective study. The left 2.5-cm subcostal incision was the sole point of entry. Data of patients who underwent SILS adrenalectomy were compared with those from an uncontrolled group of patients who underwent conventional laparoscopic adrenalectomy during the same study period.
Results
There were 20 patients in each study group (20 men, 20 women; mean age [SD] = 50 [6.5] years). SILS was successfully performed and none of the patients required conversion to an open procedure. In one case of SILS procedure, an additional lateral 5-mm port was needed for retraction of the kidney. The mean (SD) duration of the operation was 95 (20) min in the SILS group and 80 (8) min in the conventional laparoscopic adrenalectomy group (p = 0.052). There were no intraoperative or postoperative complications. There were no differences between the two study groups with respect to postoperative pain, number of patients who resumed oral intake within the first 24 h, final pathologic diagnosis, and length of hospital stay.
Conclusion
SILS left adrenalectomy is a technically feasible and safe procedure in carefully selected patients. The definitive clinical, aesthetic and functional advantages of this technique require further analysis.
Fulltext Preview
From http://www.springerlink.com/content/h60075322750m0x0/
New drug shows promise in patients with rare illness
Two in Montreal with Cushing's disease were among 16 in international trial
By AARON DERFEL, The Gazette
Quebecers suffering from Cushing's disease - a rare hormonal disorder - have some reason to be hopeful after a clinical trial conducted partly in Montreal has shown promising results of a new drug.
About 400 to 500 Quebecers have Cushing's disease or syndrome, a disorder that produces tumours on the pituitary gland, leading to a spike in cortisol levels.
The excess cortisol can cause a wide range of problems, including obesity, hypertension and diabetes as well as sleep and mood disorders.
In some people, deposits of fat accumulate on the back of the neck and shoulders, an effect known as a "buffalo hump."
Until now, surgery and radiotherapy have been the only options for many patients. However, a drug developed by Novartis Pharmaceuticals has been found to act on the tumours, cutting cortisol levels an average of 50 per cent.
In some patients - two of them from Quebec - cortisol levels returned to normal.
The drug, pasireotide, involves twice-daily injections. The treatment has yet to be approved by Health Canada.
"This study is very promising, especially for patients for whom complete surgical removal of tumours - the standard treatment for this disease - was not possible," said Dr. André Lacroix, an endocrinologist at the Centre hospitalier de l'université de Montréal.
Lacroix and his colleagues tested the drug on four patients. In addition to the two who "experienced a complete regression of all symptoms" of Cushing's disease, the two others reported drops in their cortisol levels and an improvement in their health, Lacroix noted.
The findings of the international study of 16 patients were published in the latest edition of the New England Journal of Medicine.
Pasireotide acts by binding to certain receptors on the tumours. Lacroix's team has also carried out a separate study of another drug that targets a different receptor.
He suggested that using the two drugs together might prove even more beneficial, but this must be borne out by further research.
The ideal patients for the drug therapy would be those whose tumours are too small for surgery, Lacroix said.
Each year in Quebec, there are about 15 new cases of Cushing's disease, and doctors at the CHUM treat about 150 patients.
© Copyright (c) The Montreal Gazette
Saturday, March 17, 2012
We Have Lost Another Cushie.
I don't have permission yet to post any details but suffice it to say, losing even one Cushing's patient is one too many.
We have a list of those that we know about here http://www.cushie.info/index.php?option=com_content&view=category&id=... and I'm sure that there are many more that we never hear about.
Cushing's can be fatal.
"Cushing's disease is a rare disorder, with three to five cases per million people. It can affect all ages and both genders but is most common in otherwise healthy young women," says Beverly M.K. Biller, MD, of the Massachusetts General Hospital Neuroendocrine Unit, senior author of the study. "Often misdiagnosed, Cushing's is associated with a broad range of health problems – causing physical changes, metabolic abnormalities and emotional difficulties – and if not controlled, significantly increases patients' risk of dying much younger than expected."
If you think you have Cushing's, please keep fighting as long as you need to to get help. We don't need any more names on the In Memory list!
Friday, March 16, 2012
Boston, Pituitary Day, 2012
On behalf of the Brain Science Foundation, the Department of Neurosurgery at Brigham and Women’s Hospital and the BWH Pituitary/Neuroendocrine Center, you are invited to attend Pituitary Day. This program will take place on Saturday, March 24, 2012, from 7:45 AM to 5:00 PM at the Bornstein Amphitheater at Brigham and Women’s Hospital in Boston.
Pituitary Day is a conference that unites patients, caregivers, family and friends with leading clinicians, researchers, nurses and other experts to discuss the latest in pituitary diagnosis and treatment. By way of a series of presentations and panel discussions, we will discuss basic and new information related to pituitary disorders, including physical and psychological aspects, and other important patient issues.
Our expectation is for this to be a truly remarkable and empowering experience and we hope you will consider joining us this year. For more information, please contact Sarah Donnelly at 781-239-2903 or sarah@brainsciencefoundation.org.
When
Saturday March 24, 2012 from 7:45 AM to 5:00 PM EDT
Where
Brigham & Women's Hospital, Bornstein Amphitheater
45 Francis Street
Boston, MA 02115
Experimental drug reduces cortisol levels, improves symptoms in Cushing's disease
International phase 3 trial is largest study ever of rare endocrine disorder
A new investigational drug significantly reduced urinary cortisol levels and improved symptoms of Cushing's disease in the largest clinical study of this endocrine disorder ever conducted. Results of the clinical trial conducted at centers on four continents appear in the March 8 New England Journal of Medicine and show that treatment with pasireotide cut cortisol secretion an average of 50 percent and returned some patient’s levels to normal.
"Cushing's disease is a rare disorder, with three to five cases per million people. It can affect all ages and both genders but is most common in otherwise healthy young women," says Beverly M.K. Biller, MD, of the Massachusetts General Hospital Neuroendocrine Unit, senior author of the study. "Often misdiagnosed, Cushing's is associated with a broad range of health problems – causing physical changes, metabolic abnormalities and emotional difficulties – and if not controlled, significantly increases patients' risk of dying much younger than expected."One of several conditions that lead to Cushing's syndrome – chronically elevated secretion of the hormone cortisol – Cushing's disease is caused by a benign pituitary tumor that oversecretes the hormone ACTH, inducing increased cortisol secretion by the adrenal glands. Symptoms of Cushing's syndrome include weight gain, hypertension, mood swings, irregular or absent periods, abnormalities of glucose processing – insulin resistance, glucose intolerance and type 2 diabetes – and cardiovascular disease. Since those symptoms are associated with many health problems, physicians may not consider the rare possibility of Cushing's. The diagnosis can be difficult to make and usually requires the expertise of an endocrinologist. Since cortisol levels normally fluctuate during the day, a single blood test probably would not identify chronic elevation, so the most common diagnostic test measures a patient's 24-hour urinary output. First-line treatment for Cushing's disease is surgical removal of the ACTH-secreting tumor, which can lead to remission in 65 to 90 percent of patients who are treated by expert pituitary surgeons. But symptoms return in 10 to 30 percent of those patients, requiring repeat surgery, radiation therapy or treatment with drugs that interfere with part of the cortisol control system. Until last month, there was no specific FDA-approved medical treatment for Cushing's syndrome; and while the newly approved drug mifepristone should benefit some patients, it does not affect the pituitary source of the condition or reduce cortisol levels. The current phase 3 trial of pasireotide – the first drug that blocks ACTH secretion by binding to somatostatin receptors on the pituitary tumor – was sponsored by Novartis Pharma and enrolled 162 patients at 62 sites in 18 countries. Almost 85 percent of participants had either persistent disease that had not responded to surgery or had recurrent disease. The other 15 percent were recently diagnosed but not appropriate candidates for surgery. Participants were randomly assigned to two groups, one starting at two daily 600-microgram injections of pasireotide, the other receiving 900-microgram doses. Three months into the 12-month trial, participants whose urinary cortisol levels remained more than twice the normal range had their dosage levels increased. During the rest of the trial, dosage could be further increased, if necessary, or reduced if side effects occurred. At the end of the study period, many patients had a significant decrease in their urinary cortisol levels, with 33 achieving levels within normal range at their original dosage by month 6 of the trial. Participants whose baseline levels were less than five times the upper limit of normal were more likely to achieve normal levels than those with higher baseline levels, and the average urinary cortisol decrease across all participants was about 50 percent. Many Cushing's disease symptoms decreased, and it became apparent within the first two months whether or not an individual was going to respond to pasireotide. Transient gastrointestinal discomfort, known to be associated with medications in the same family as pasireotide, was an expected side effect. But the investigators observed elevated glucose levels in 73 percent of participants, something not seen to the same extent with other medications in this family. That will require close attention, since many Cushing's patients already have trouble metabolizing glucose. Biller explains, "Those patients who already were diabetic had the greatest increases in blood sugar, and those who were pre-diabetic were more likely to become diabetic than those who began with normal blood sugar. However, elevations were even see in those who started at normal glucose levels, so this is real and needs to be monitored carefully." Additional trials of pasireotide are in the works, and a phase 3 study of a long-acting version of the drug was recently announced. Biller notes that the potential addition of pasireotide to available medical treatments for Cushing's disease would have a number of advantages. "It's very important to have medications that work at different parts of the cortisol control system – which is the case for the currently used medications that work at the adrenal gland level, pasireotide which works at the pituitary gland, and mifepristone which blocks the action of cortisol at receptors in the body. Having more options that work in different ways is valuable because not all patients respond to one medicine and some may be unable to tolerate a specific drug's side effects. "As we have more drugs available to treat Cushing’s," she adds. "I think in the long run we may start using combinations of drugs, which is the approach we use in some patients with acromegaly, another disorder in which a pituitary tumor causes excess hormone secretion. Ultimately we hope to be able to give lower doses leading to fewer overall side effects, but that remains to be determined by future studies." Biller is a professor of Medicine at Harvard Medical School. Annamaria Colao, MD, PhD, University of Naples, Italy, is the lead author of the New England Journal report. Additional co-authors are Stephan Petersenn, MD, University of Duisberg-Essen, Germany; John Newell-Price, MD, PhD, University of Sheffield, U.K.; James Findling, MD, Medical College of Wisconsin, Milwaukee; Feng Gu, MD, Peking Union Medical College Hospital, Beijing, China; Mario Maldonado, MD, Ulrike Schoenherr, Dipl-Biol, and David Mills, MSc, Novartis Pharma; and Luiz Roberto Salgado, MD, University of São Paulo Medical School, Brazil. Massachusetts General Hospital, founded in 1811, is the original and largest teaching hospital of Harvard Medical School. The MGH conducts the largest hospital-based research program in the United States, with an annual research budget of more than $750 million and major research centers in AIDS, cardiovascular research, cancer, computational and integrative biology, cutaneous biology, human genetics, medical imaging, neurodegenerative disorders, regenerative medicine, reproductive biology, systems biology, transplantation biology and photomedicine.From http://www.massgeneral.org/about/pressrelease.aspx?id=1444#.T2I2Ue9AMtQ.facebook
Interview with Leiana, Adrenal Patient
Leiana was diagnosed with autoimmune adrenal insufficiency in 2009 and put on 30mg of Cortef for the rest of her life. Her cortisol levels were below normal of -1. She has been trying to wean off the steroids with no success.
She had a 3.9 adenoma on the right adrenal gland removed in Sept 2010 is waiting for the left adrenal gland to kick in. She is extremely skinny and bony and eats around 3000 to 4000 calories a day.
Read Leiana's bio here.
Listen Live at http://www.blogtalkradio.com/CushingsHelp
The Call-In number for questions or comments is (646) 200-0162.
Archives will be available after the interview
Wednesday, March 14, 2012
Retroperitoneal Adrenal-Sparing Surgery for the Treatment of Cushing's Syndrome Caused by Adrenocortical Adenoma: 8-Year Experience With 87 Patients
Hong-chao He, Jun Dai, Zhou-jun Shen, Yu Zhu, Fu-kang Sun, Yuan Shao, Rong-ming Zhang, Hao-fei Wang, Wen-bin Rui and Shan Zhong
Abstract
Background
The objective of this study was to present our 8-year experience with partial adrenalectomy via the retroperitoneal approach for the treatment of Cushing’s adenoma.
Methods
A total of 93 patients who underwent adrenal surgery for Cushing’s adenoma from March 2003 to December 2010 were enrolled in this study. Preoperative, intraoperative, and postoperative variables were reviewed from the database. Student’s t test was used to analyze the continuous data, and the χ2 test was used to analyze the categoric data. A value of p < 0.05 was considered statistically significant.
Results
Adrenal-sparing surgery was performed in 87 cases (31 by open surgery, 56 by retroperitoneal laparoscopy). Six patients underwent open/laparoscopic total adrenalectomy because of recurrent disease or a large size. The cure rate in our series was 97.8%. Hypertension resolved in 34 of 64 patients (53.1%), diabetes in 7 of 27 patients (25.9%) and obesity in 28 of 48 patients (58.3%). One patient died during the postoperative period. The intraoperative complication rate for the open surgery group was significantly higher than that for the retroperitoneal laparoscopy group (9.1 vs. 1.7%).
Conclusions
The retroperitoneal approach is reliable and safe for treating Cushing’s syndrome. The laparoscopic technique can decrease the prevalence of intraoperative complications. Retroperitoneal laparoscopic partial adrenalectomy can be performed with extremely low morbidity and achieves an excellent outcome, although death may occur during the postoperative period in high-risk patients. Postoperative management plays an important role in the surgical treatment of Cushing’s syndrome.
Jun Dai is listed as co-first author.
From http://www.springerlink.com/content/034754537j7586k2/
Tuesday, March 13, 2012
The Adrenal Vein Sampling International Study (AVIS) for Identifying the Major Subtypes of Primary Aldosteronism
- Gian Paolo Rossi,
- Marlena Barisa,
- Bruno Allolio,
- Richard J. Auchus,
- Laurence Amar,
- Debbie Cohen,
- Christoph Degenhart,
- Jaap Deinum,
- Evelyn Fischer,
- Richard Gordon,
- Ralph Kickuth,
- Gregory Kline,
- Andre Lacroix,
- Steven Magill,
- Diego Miotto,
- Mitsuhide Naruse,
- Tetsuo Nishikawa,
- Masao Omura,
- Eduardo Pimenta,
- Pierre-François Plouin,
- Marcus Quinkler,
- Martin Reincke,
- Ermanno Rossi,
- Lars Christian Rump,
- Fumitoshi Satoh,
- Leo Schultze Kool,
- Teresa Maria Seccia,
- Michael Stowasser,
- Akiyo Tanabe,
- Scott Trerotola,
- Oliver Vonend,
- Jiri Widimsky Jr.,
- Kwan-Dun Wu,
- Vin-Cent Wu and
- Achille Cesare Pessina
-Author Affiliations
- University of Padova (G.P.R., M.B., T.M.S., A.C.P.), Department of Medicine (DIMED) Internal Medicine 4, Padova, 35128 Italy; University Hospital Würzburg (B.A.), Department of Internal Medicine I, Endocrine and Diabetes Unit, Würzburg, 97080 Germany; University of Texas (R.J.A.), Southwestern Medical Center at Dallas, Dallas, Texas 75390; Hôpital Européen Georges Pompidou (L.A., P.-F.P.), Hypertension Unit, Paris, 75908 France; Hospital of The University of Pennsylvania (D.C.), Department of Internal Medicine, Philadelphia, Pennsylvania 19104; University Hospital Innenstadt (C.D.), Department of Clinical Radiology, Munich, 80336 Germany; Radboud University Nijmegen (J.D.), Department of Internal Medicine, Nijmegen, 6225GA Netherlands; University Hospital Innenstadt (E.F., M.R.), Department of Endocrinology, Munich, Germany; University of Queensland School of Medicine (R.G., E.P., M.S.), Greenslopes Hospital, Endocrine Hypertension Research Centre, Brisbane, 4120 Australia; University Hospital Würzburg (R.K.), Institute of Radiology, Würzburg, Germany; University of Calgary (G.K.), Foothills Medical Centre, Calgary, T2N4J8 Canada; Centre hospitalier de l'Université de Montréal (A.L.), Department of Medicine, Montreal, H2W 1T8 Canada; Medical College of Wisconsin (S.M.), Endocrinology Clinic Community Memorial Medical Commons, Menomonee Falls, Wisconsin 53051; University of Padova (D.M.), Department of Medicine (DIMED) Radiology, Padova, Italy; National Hospital Organization Kyoto Medical Center (M.N.), Department of Endocrinology Clinical Research Institute, Kyoto, 612-8555 Japan; Yokohama Rosai Hospital (T.N., M.O.), Department of Endocrinology and Metabolism, Yokohama City, 222-0036 Japan; Clinical Endocrinology (M.Q.), Charité Campus Mitte, Charité University Medicine Berlin, Berlin, 10117 Germany; Azienda Ospedaliera Santa Maria Nuova (E.R.), Department of Internal Medicine, Reggio Emilia, 42123 Italy; Department of Nephrology (L.C.R., O.V.), Heinrich-Heine-University Düsseldorf, Düsseldorf, 40225 Germany; Tohoku University Hospital (F.S.), Department of Nephrology, Endocrinology and Vascular Medicine, Sendai, 980-8574 Japan; Department of Radiology (L.S.K.), Radboud University Nijmegen Medical Center, Nijmegen, Netherlands; Institute of Clinical Endocrinology (A.T.), Tokyo Women's Medical University, Tokyo, 162-8666 Japan; Hospital of The University of Pennsylvania (S.T.), Department of Radiology, Philadelphia, Pennsylvania; Charles University in Prague (J.W.), General Faculty Hospital, Third Department of Medicine, Prague, 12808 Czech Republic; and National Taiwan University Hospital (K.-D.W., V.-C.W.), Department of Internal Medicine, Taipei, 10048 Taiwan
- Address all correspondence and requests for reprints to: Prof. Gian Paolo Rossi, M.D., FACC, FAHA, Department of Medicine, Internal Medicine 4, University Hospital via Giustiniani, 2, 35126 Padova, Italy. E-mail: gianpaolo.rossi@unipd.it.
Abstract
Context: In patients who seek surgical cure of primary aldosteronism (PA), The Endocrine Society Guidelines recommend the use of adrenal vein sampling (AVS), which is invasive, technically challenging, difficult to interpret, and commonly held to be risky.
Objective: The aim of this study was to determine the complication rate of AVS and the ways in which it is performed and interpreted at major referral centers.
Design and Settings: The Adrenal Vein Sampling International Study is an observational, retrospective, multicenter study conducted at major referral centers for endocrine hypertension worldwide.
Participants: Eligible centers were identified from those that had published on PA and/or AVS in the last decade.
Main Outcome Measure: The protocols, interpretation, and costs of AVS were measured, as well as the rate of adrenal vein rupture and the rate of use of AVS.
Results: Twenty of 24 eligible centers from Asia, Australia, North America, and Europe participated and provided information on 2604 AVS studies over a 6-yr period. The percentage of PA patients systematically submitted to AVS was 77% (median; 19–100%, range). Thirteen of the 20 centers used sequential catheterization, and seven used bilaterally simultaneous catheterization; cosyntropin stimulation was used in 11 centers. The overall rate of adrenal vein rupture was 0.61%. It correlated directly with the number of AVS performed at a particular center (P = 0.002) and inversely with the number of AVS performed by each radiologist (P = 0.007).
Conclusions: Despite carrying a minimal risk of adrenal vein rupture and at variance with the guidelines, AVS is not used systematically at major referral centers worldwide. These findings represent an argument for defining guidelines for this clinically important but technically demanding procedure.
- Received October 14, 2011.
- Accepted January 31, 2012.
- Copyright © 2012 by The Endocrine Society
From http://jcem.endojournals.org/content/early/2012/03/01/jc.2011-2830.abstract?rss=1